INTRODUCTION
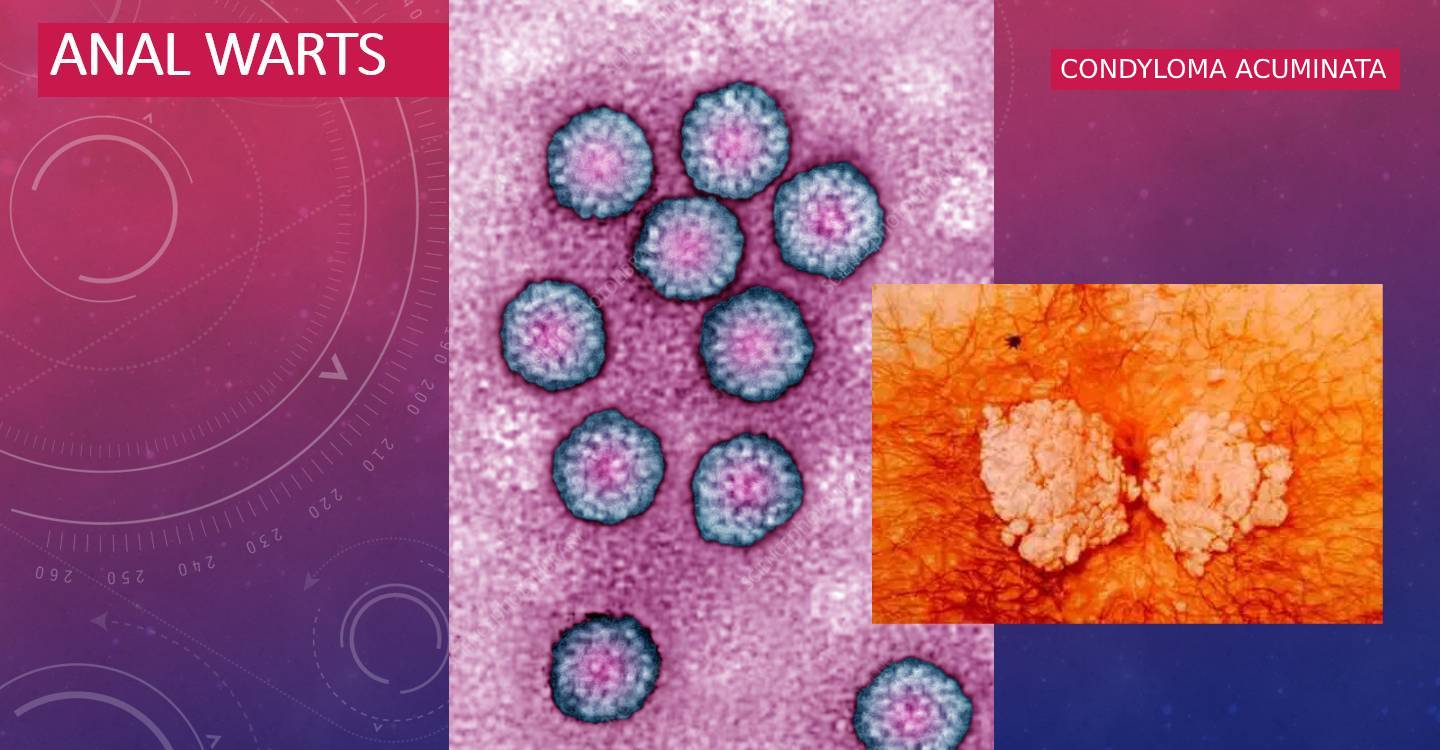
Anal or ano-genital warts also known as condyloma acuminata is caused by Human papilloma virus (HPV).
The infection due to this virus is restricted to humans and is the most common Sexually transmitted infection.(STI)
Sexually active people have at least a 50% risk of becoming infected at least once in their lifetime, if they are not vaccinated.
Around 90% of these infections are asymptomatic & self-limiting because the immune system clears most infection within 2 years.
There are more than 40 different types of HPVs that can cause STIs . Out of these only few have the potential to cause ano -genital cancers.
Low-risk HPV types include HPV types 6 and 11, and these are the most common etiologic agents for genital warts, while the high-risk HPV types 16 and 18 are associated with cancers of the anus, cervix, penis, vulva, and vagina. Genital warts may also harbor more high-risk HPV types 16, 18, 31, 33, and 35 and may contain areas of high-grade dysplasia.
MODE OF INFECTION AND SPREAD:
The primary mode of transmission of of anogenital HPV infection is sexual intercourse , although spread may occur via non sexual intimate contacts thus accounting for rare occurance of these infections in virginal women and children.
This is accomplished by fluid transfer containing shed viral particles from someone having anal condyloma.
Upto 30% of sexually active people harbor HPV under fingernails as one mode of spread.
Trauma to the perianal epithelium during intercourse leads to inoculation of viral particles in the basal layer cells of the skin where the virus replicates. When the cells migrate to more superficial layers , infective particles are released in the form of visible warts.
Mature infectious particles are found in the surface layers of the lesions.
The combination of moisture, maceration, and tiny epithelial defects seems to facilitate the transfer of HPV.
Patients with atopic dermatitis, contact dermatitis, and other forms of dermatitis are also at greater risk. Patients with impaired resistance - HIV/AIDS ,chemotherapy, long-term immunosuppressive therapy - are also more susceptible. Underlying systemic diseases such as diabetes mellitus and malignancies may also play a role.
The incubation period is highly variable ranging from several weeks to years. This time span indicates that the HPV rapidly infects host epithelial cells, but that they may lie dormant for a variable period of time before altering the proliferation of the host cell.
Condylomata acuminata may spontaneously disappear. They might as well persist and progress over years into a large destructive tumor, the Buschke-Lowenstein tumor.
DIAGNOSIS
The diagnosis is usually made on inspection alone, by the Proctologist. Examination typically reveals pinkish warts of varying sizes that may coalesce to form a mass
Endoscopic examination of the anal acanal & rectum is recommended to identify and treat internal lesions which can serve as a source of re-infection and to monitor for the possibility of anal carcinoma.
High resolution anoscopy with the application of acetic acid improves detection rate. In addition, typical accompanying diseases such as gonorrhea, syphilis, and HIV/AIDS should be excluded. When clinical signs are present, candidiasis, trichomoniasis, and oxyuriasis should also be excluded.
Histopathology examination confirms the diagnosis. The classic microscopic findings include koilocytes in the upper layers of the epithelium ,acanthosis and papillomatosis.
A tissue specimen can be useful for HPV typing. HPV 6 and 11 are classified as carcinogenic but low-risk, while HPV 16, 18, and 31 are considered high-risk. Clinical distinction is impossible.
DIFFERENTIAL DIAGNOSIS: The differential diagnostic considerations vary depending on the location, but include the following disorders: Verrucae vulgares, Bowenoid papulosis, Bowen disease, Condylomata lata (secondary syphilis), Mollusca contagiosa, Pemphigus vegetans, Squamous cell carcinoma. Paget disease Seborrheic keratoses, Lichen planus.
CLINICAL PRESENTATION
Ano genital warts, or condyloma, present as growths on the genital mucosa, anal mucosa, and perianal skin.
Symptoms may include pain, pruritus (itchiness), discharge, bleeding, discomfort, depending on the location and size of the warts.
Large wart may block the anal canal orifice.
Whitening occurs on applying acetic acid on it.
Three clinical types have been identified -
Condylomata acuminata: papillomatous or filiform lesions which typically arise in the anogenital region
Condylomata plana: flatter lesions most common on the prepuce and cervix
Condylomata gigantea (Buschke-Lowenstein tumor): now considered a verrucous carcinoma.
Condylomata acuminata are typically found in moist body folds, such as around the genitalia or in the perianal region.
They can occasionally extend into the rectum or urethra. Similar lesions are found in the mouth, as well as in other occluded sites such as the axillae, umbilicus, and inframammary region. vulvae. The clinical appearance of condylomata acuminata is determined by the terrain in which they grow. For example, condylomata acuminata which grow in the gluteal cleft with pressure on both sides from the buttocks, often develop as a hyperkeratotic linear ridge, known in German as a "rooster comb lesion" when there is less mechanical pressure, they tend to have a cauliflower-like appearance.
THERAPY
Since condylomata acuminata have a low spontaneous remission rate, can develop into malignancies, and are often sexually transmitted, all lesions should be treated as soon as they are identified.
The mainstay of treatment for smaller lesions is podophyllotoxin.
0.5% commercial podophyllotoxin preparation (Condylox) is recommended. The standard regimen is to paint the solution on the lesions b.i.d. for 4 days, then rest for 3-10 days and then re-institute therapy. Podophyllotoxin only works well on moist, macerated, or mucosal lesions. To be used under guidance of specialist only.
Imiquimod cream 5% is a promising new therapy option. It is a topical immunomodulatory agent which stimulates a spectrum of cytokines in the skin. Typically, it is applied three times weekly until healing or for a maximum of 16 weeks).
Topical 5- fluorouracil cream is another treatment option.
A useful adjuvant approach for patients with extensive disease is the injection of interferon. It is administered systemically or intralesional or sublesional. A topical interferon-j3 gel is available in Europe for application following surgical or laser removal of the lesions . It is crucial to ensure that the sexual partner(s) of the patient are examined and treated, as appropriate. Often, the partner will have an asymptomatic infection. If a man has penile condylomata acuminata, his female partner surely deserves evaluation to exclude cervical disease. Both individuals then require long-term follow-up because of the likelihood of recurrence and the risk of malignant disease
Other useful treatment options are laser destruction, curettage, and cautery, or other electrosurgical removal.
In our clinic we perform LASER & Radiofrequency destruction of lesions under local anesthesia cream. It is a painless and bloodless procedure with immediate disappearance of the lesions.
Extensive disease as well as anal canal lesions are treated as a DAYCARE procedure under General Anesthesia or regional block. Since recurrence rate is significant, close follow-up of patients is advised.