INTRODUCTION
Anorectal abscess is a collection of pus due to infection in relation to the anal canal & Rectum and surrounding soft tissues.
Though common in Diabetics and immunosuppressed it can affect healthy individuals. 95% of anorectal abscesses are due to infection of the anal glands in relation to crypts- cryptoglandular disease.
Since it is a cryptoglandular infection, almost 50% of anorectal abscesses persist as a chronic process known as Anal fistula. It is also called as fistulous abscess where Abscess represents an acute phase , while fistula represents a chronic phase.
The incidence of abscess is reportedly between 0.4% and 5% of patients undergoing operative management.
The condition is more common in males as compared to females.
The most common causative organism cultured from the pus is E. coli (60%).
Other causative organisms are Staphylococcus, Streptococcus, B.proteus, Bacteroides.
The condition presents as acute onset of anal pain with or without a visible swelling and must be treated urgently to avoid spread of infection in the tissues surrounding anorectum as well as to minimise the possibility of fistula formation.
Causes of ANORECTAL ABSCESS
In the middle portion of the anal canal at the level of the dentate line, the ducts of the anal glands empty into the anal crypts. The greatest concentration of these glands is in the posterior aspect of the anal canal.
Obstruction of these ducts, whether secondary to fecal material .foreign bodies, or trauma, results in stasis and infection & hence abscess formation.
Predisposing factors include liquid stool entering the anal duct, trauma, tobacco abuse, and cystic dilation of the duct resulting in poor emptying. The remaining few are the result of specific disorders such as inflammatory bowel disease (IBD), and malignancy.
Other causes :
- Injury to anorectum
- Cutaneous infection ( Boil) .
- Blood borne infections.
- Anal fistulas
- Fissure in ano
- Perianal hematoma
- Post-anorectal Surgery
- Crohn’s disease
- Tuberculosis
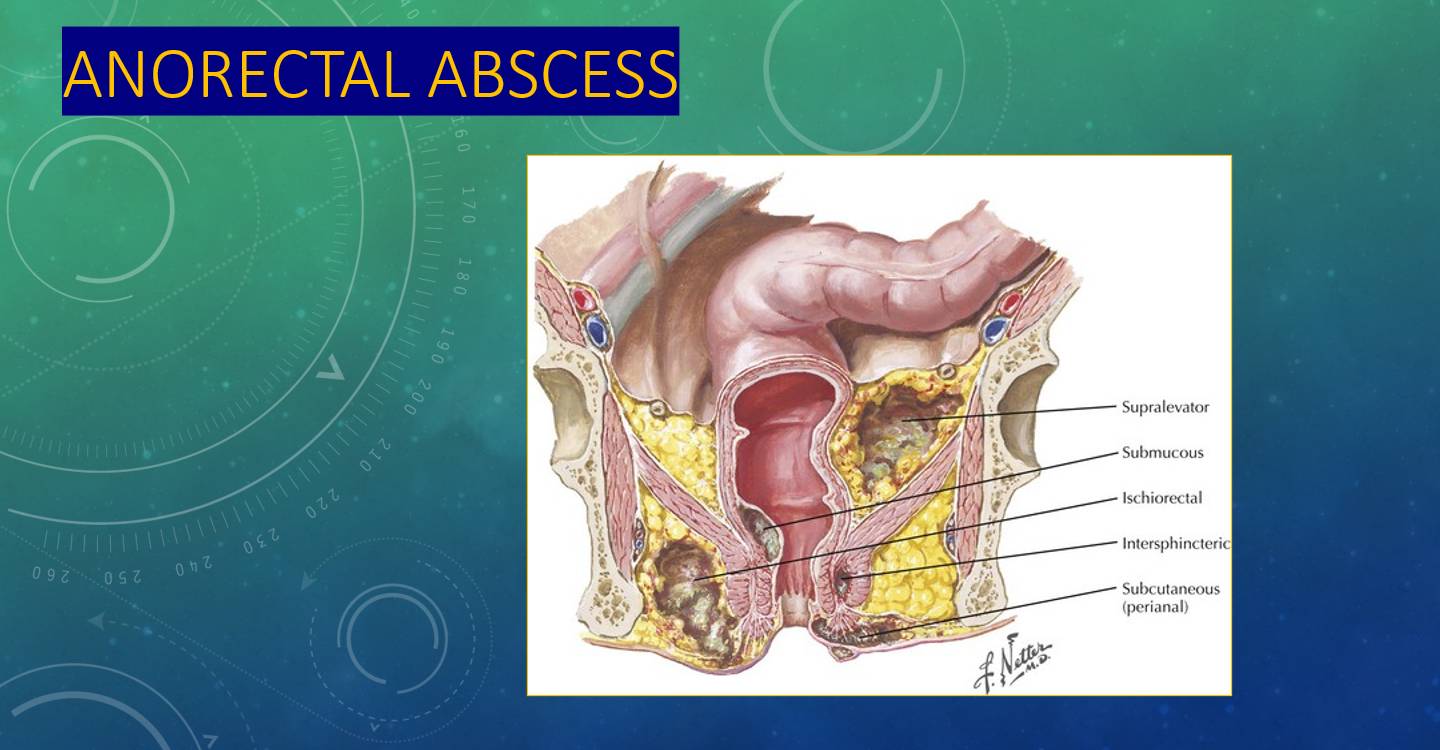
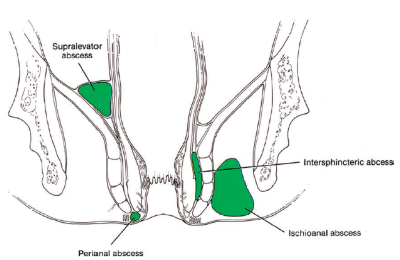
TYPES OF ANO RECTAL ABSCESS
- PERIANAL ABSCESS
- ISCHIORECTAL ABSCESS
- SUBMUCOUS ABSCESS
- INTERSPHINCTERIC ABSCESS
- SUPRALEVATOR ABSCESS
- FISSURE ABSCESS
Perianal abscess (60%)
- It occurs due to infection of anal glands in the perianal region.
- It may be due to a boil, anal gland infection or thrombosed external pile.
- It produces severe anal pain, throbbing in nature and on examination a soft, tender, warm swelling is found at the anal verge.
- Rectal examination reveals a tender, boggy, swelling under the anal mucosa


lschiorectal abscess (30%)
- Collection of pus in the ischiorectal fossa, which is lateral to rectum and medial to pelvic wall.
- Bounded above by levator ani and inferiorly by pad of fat in the ischiorectal fossa.
- lschiorectal fat is poorly vascularised. Hence, it is more vulnerable to infection.
- Abscess occurs due to spread of perianal abscess or due to blood-borne infection. Fossa communicates with that of opposite side through post-sphincteric space and so horse-shoe like abscess can occur.
- Diabetes is the precipitating factor
Submucous abscess (5 %)
Collection of pus under the mucous membrane of rectum or anal canal. There is no obvious swelling externally.
• It can also be due to infection of injected haemorrhoids.
Pelvirectal Abscess
It is situated between the upper surface of levator ani and pelvic peritoneum. Pelvic and supralevator
abscesses are uncommon and may result from extension of an intersphincteric or ischiorectal abscess upward or extension of an intraperitoneal abscess downward. It is almost like a pelvic abscess, occurs secondary to appendicitis, salpingitis, diverticulitis, Crohn’s.
Intersphincteric abscesses occur in the intersphincteric space and are notoriously difficult to diagnose, often requiring an examination under anesthesia. Pus collects between the internal and external sphincters and may spread upwards to supralevator space or downwards to form perianal abscess.
CLINICAL FEATURES
There is severe pain in the anal region. Patient is unable to sit in a chair due to severity of pain.
In early phase of perianal abscess, there is just a redness of the skin with tenderness in the perianal region.
Soon a tender swelling appears in perianal region. Apart from having severe pain, the patient might have high fever and urinary retention.
An ischiorectal abscess causes diffuse swelling in the ischiorectal fossa that may involve one or both sides, forming a “horseshoe” abscess.
Intersphincteric abscesses produce little swelling and few perianal signs of infection. Pain is typically described as being deep and “up inside” the anal area and is usually exacerbated by coughing or sneezing.
A submucous abscess might spontaneously rupture with discharge of pus through the anus.
Diagnosis :
The diagnosis of a perianal or ischiorectal abscess can usually be made with physical exam alone (either in the office or in the operating room). Digital rectal examination is very painful and avoided in most of the cases.
Intersphincteric abscesses are notoriously difficult to diagnose because they produce little swelling and few perianal signs of infection. They are diagnosed by high index of suspicion and imaging.
Because of its proximity to the peritoneal cavity, supralevator abscesses can mimic intra-abdominal conditions. Digital rectal examination may reveal an indurated, bulging mass above the anorectal ring.
Submucous abscess presents as aching pain in the anorectum with significant perineal discomfort.
On digital examination (P/R), there is a palpable tender, soft, smooth swelling in the lower rectum and anal canal.
It may be missed clinically as there is no obvious swelling externally.
Differential diagnosis of anorectal abscesses :
- Hidradenitis suppurativa
- Pilonidal abscess
- Tuberculosis
- Actinomycosis
Investigations
- MRI is the investigation of choice for anorectal abscess.
- Perineal and anal US is also very useful.
- Investigations relevant to specific cause may be done.
- Proctosigmoidoscopy is needed to identify secondary cause in anorectum.
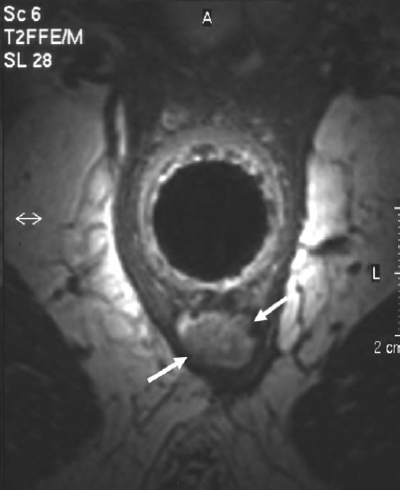
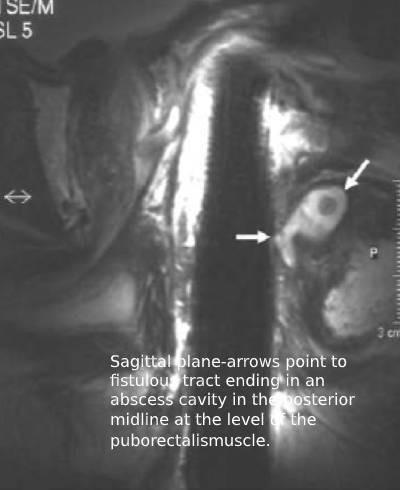
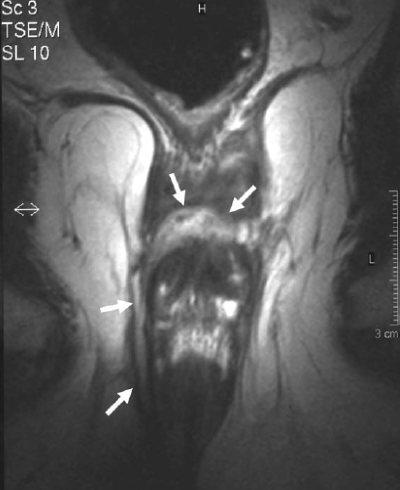
MRI scan is especially useful when there are no external signs of, but a high index of suspicion of anorectal abscess. It is also indicated in a complex fistulous abscess.
TREATMENT OF ANORECTAL ABSCESSES
Prompt surgical drainage and debridement of the abscess is the cornerstone of any abscess management.
Antibiotics has a lesser role and only indicated when associated cellulitis is present, in patients who fail to improve following appropriate drainage, and those with immunosuppressed states.
Incision and drainage :
It depends on the location of abscess and the experience of surgeon. external drainage is done by cruciate incision over the prominence of abscess with excision of skin edges to prevent premature closure of the cavity. Incision must be always close to the anal verge so that if fistula develops it will be easily manageable.
candidates for internal drainage via anal canal or rectum include (1) submucosal abscess, (2) intersphincteric abscess, (3) supralevator abscess from intersphincteric fistula, and (4) supralevator abscess from pelvic disease.
Supralevator abscesses require delineation of the track by imaging before surgical correction is undertaken. When the inciting source is intra-abdominal, transrectal drainage is indicated in most scenarios. However, abdominal drainage can be considered depending upon ease of access and directionality of the abscess cavity. When the source is intraabdominal, percutaneous management may prevent creation of a fistulous track through the levator plate via improper ischiorectal drainage
Catheter Drainage
Minimization of perianal incisions is possible using the placement of a drainage catheter within the abscess cavity
Indicated especially in
- patients with large abscess cavities,
- patients with severe systemic illness,
- those with underlying comorbidities including diabetes
- mellitus and morbid obesity.


HORSESHOE ABSCESS
These are managed by Hanley’s procedure or modified Hanley’s procedure where the abscess is openly drained through anococcygeal ligament and counter incisions over both ischiorectal fossae to control the lateral tracts.
If necessary, a seton (cutting or noncutting) is placed in the posterior midline, with subsequent definitive management taking place at a later time.
Post operative care
- Local wound care involves sitz baths two to three times daily followed by wound coverage using gauze.
- Following catheter drainage ,a dressing is similarly applied over the catheter end to prevent soiling of clothing.
- Surgeon follow-up is indicated at 2–3 weeks or earlier in patients who undergo incision and drainage, and 7–10 days in those with mushroom-tip catheters. Endpoint for removal is cessation of purulent drainage from the drain, and closure of the wound around catheter.
- Antibiotics are not warranted in the postoperative setting unless cellulitis is present, or in the immunocompromised patient.
- Analgesics are given for pain control
- Bulk forming fibre supplements are given in first month to help in easy stool passage.

Sitz bath after surgery for anorectal abscess,fistula,piles, fissure .Antiseptic solution is mixed in Warm water at 42 degree Celsius . Patient is asked to sit for 15-20 minutes 2-3 times per day ( especially after passing stools )