
- Rectal prolapse is defined as protrusion of the rectum out of anal opening.
- Rectal prolapse is complete when full- thickness of rectal wall prolapse out of anal canal.
- If the rectal wall does not protrude out, it is called an occult (internal) rectal prolapse.
- Mucosal prolapse is one in which there is protrusion of only rectal mucosa.
Rectal prolapse is Telescoping of the Rectum out of Anus.
The description of the rectal prolapse was first noted on papyrus in 1500 BC .
It is one of the common socially distressing conditions in elderly patients particularly, the elderly female with pelvic floor dysfunction.
The male to female ratio in adult is 1:6 . The ratio is equal in children. Rectal prolapse is common between fourth and seventh decade and is seen more in females than males in their extremes of age .
- Patients who are more than 50 years of age have a six fold increased risk of having a rectal prolapse.
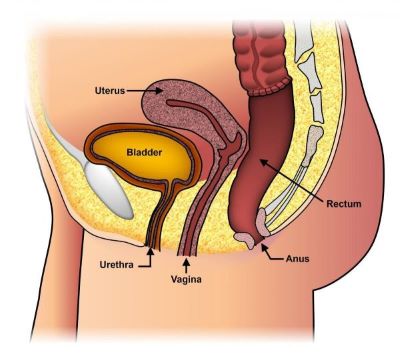
- Rectal prolapse is commonly associated with the pelvic floor descent and prolapse of bladder or uterus.
- It is usually associated with multiple pregnancies although in 35% of the cases it can be seen in nulliparous women.
- In about 50% to 75% and 25% to 50% cases, rectal prolapse is associated with fecal incontinence and constipation respectively.
- The exact aetiology of rectal prolapse is not known.
- However there are two theories :
- The first theory postulates that rectal prolapse is a sliding hernia through a defect in the pelvic fascia. This is based on the observation these patients have redundant sigmoid colon, deep peritoneal–pelvic cul de sac, diastasis of levator ani muscles, loss of posterior rectal fixation, loss of usual anorectal angle.
- The second theory holds that rectal prolapse starts as a circumferential internal intussusception of the rectum beginning 6-8 cm proximal to the anal verge. This is based on the fact of similarities in manometric findings between rectal prolapse, recto anal intussusception & solitary rectal ulcer syndrome.
- Mucosal prolapse occurs when the connective tissue attachments of the rectal mucosa are loosened and stretched, thus allowing the tissue to prolapse through the anus. This often occurs as a continuation of long-standing hemorrhoidal disease.
- Theory of perineal nerve injury was first proposed by Parks et al.
- This injury results in weakness of the pelvic floor as well as fecal incontinence. It is usually seen in patients with
- Previous history of vaginal delivery
- Excessive straining due to chronic constipation
- Patient with pelvic floor descent
- Other causes are –Inertia of the pelvic floor muscles
- Relaxation of lateral ligaments
DIFFERENTIAL DIAGNOSIS

PROCIDENTIA
Double wall circumferencetial folds
Resting and squeeze pressure

MUCOSAL PROLAPSE
Mucosa and submucosa < 4cm
Normal or Decreased
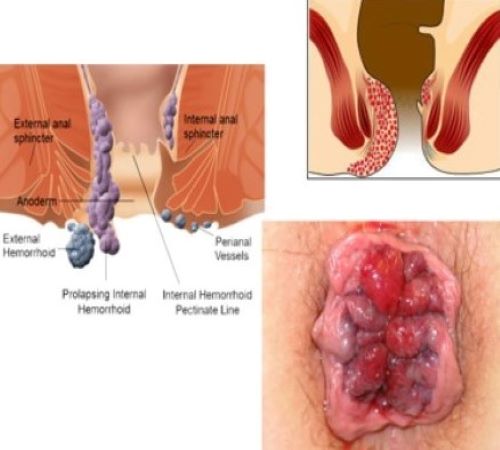
PROLAPSED HEMORRHOIDS
Radial tissue folds
Normal Resting Sphincter Pressure
Risk factors associated with increased intra-abdominal pressure
- Chronic constipation
- Benign prostatic hypertrophy, urethral strictures, bladder stones,
- Chronic obstructive pulmonary disease
- Chronic cough
- Pregnancy
- Long continued straining efforts at stool in sitting posture
- Diarrhea
- Parasitic infections like schistosomiasis and amoebiasis
- Risk factors related to local pathology
- Pelvic floor dysfunction
- Associated intraluminal rectal lesions
- Rectal adenocarcinoma
- Rectal polyp
- Malignant gastrointestinal stromal tumors
- Solitary rectal ulcer syndrome
Risk factors for anal sphincter weakness
- Diseases or injury to the brain and spinal cord
- Protracted illness, Psychiatric disease
- Previous perineal surgery
- Pelvic trauma
- Neurological diseases –
- Cauda equina syndrome
- Multiple scleroses and
- Spinal tumors
CLINICAL FEATURES
- Protruding mass out of Anus.
- In females ,associated prolapse of uterus from vagina .
- Asssociated urinary incontinence.
- Chronic straining , sensation of anorectal blockage, need of digital evacuation.
- Mucus discharge & Itching.
- Rectal bleeding.
- Constipation/ Fecal incontinence.
- Soilage.
- Feeling of incomplete evacuation.
Most often rectal prolapse is a clinical diagnosis.
Signs of rectal prolapse are:
- Protruding rectal mucosa
- Patulous anus with decreased anal tone
- Concentric and thick mucosal folds of protruding mass.
- Absence of sulcus between rectum and anal canal
Presence of solitary rectal ulcer (10-25%).
Associated bladder or uterus prolapse.
When it is not obvious in lateral decubitus position, ask the patient to sit on a commode and bear down
Investigations
- COLONOSCOPY
- COLONIC TRANSIT STUDY
- VIDEO DEFECOGRAPHY
- DYNAMIC MRI DEFECOGRAPHY
- ENDOANAL ULTRASOUND ( EAUS )
- PUDENDAL NERVE MOTOR LATENCY STUDY
- ANORECTAL MANOMETRY STUDY
- Children, are usually managed non-surgically by correcting the underlying conditions.
- Adult patients need to undergo some or other form of surgery
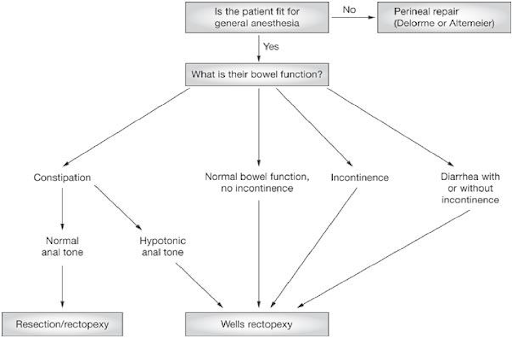
*Selection of the procedure depends upon
- patients age,
- underlying co-morbid conditions
- functional status.
Non-operative methods
- Correction of constipation
- Perineal exercises
- Electrical stimulation
- Submucosal injection of Phenol in almond oil
- Infrared coagulation
- Reduction of prolapsed rectum with gentle digital pressure
- Adhesive strapping of the buttocks
MANAGEMENT OF ACUTE IRREDUCIBLE RECTAL PROLAPSE
- Reduction under general anesthesia to relax the sphincter
- Trendelenburg position.
- Tapping the buttocks together
- Placement of sugar/salt on the prolapsed part to reduce edema
- Injection of hyaluronidase
- If prolapsed rectum is not viable, then resection of the part
Surgical treatment for prolapsed rectum
AIMS
- To control the prolapse
- To restore continence of anal sphincter
- To prevent constipation
GOALS OF SURGERY
- Narrowing of anal orifice
- Obliteration of pouch of douglas
- Restoration of pelvic floor
- Bowel resection
- Suspension/ fixation of the rectum to sacrum
- Combination of the above procedures
Surgical management
- Thiersch’s procedure of Anal Encirclement
- Delorme’s procedure
- Altemeier’s procedure
ABDOMINAL PROCEDURES
- Well’s posterior mesh rectopexy
- Ripstein anterior mesh rectopexy
- Resection rectopexy-Frykman Goldberg procedure
- Suture rectopexy
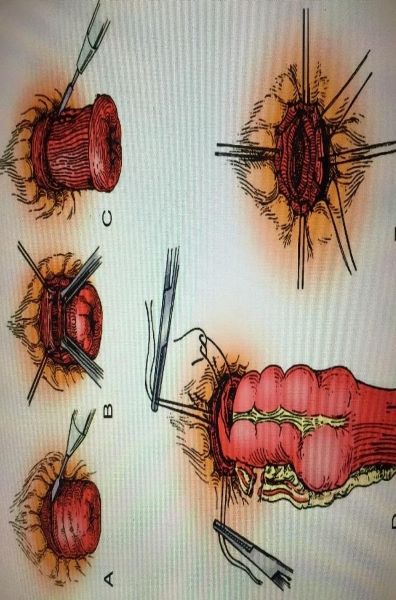
Delorme procedure
First described in 1900, by Delorme in France.
Perineal approach
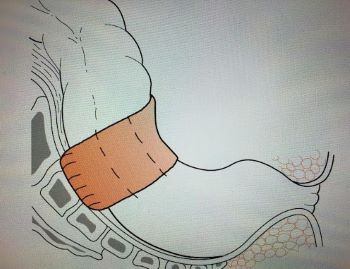
Resection of mucosa of prolapsed part.
Plication of the muscularis propria.
Mucosa to mucosa anastomosis done
Indicated in:
- Patients with small rectal prolapse.
- Patients with very high risk.
- To avoid risk of nerve damage
High Recurrence rate- 4 % - 33%
Low mortality, 0% - 2.5%.
Complications of delorme’s procedure
Largest study done by Lieberth and colleagues-
76 patients with mean age 74 years followed for 36 months
- No perioperative mortality
- Urinary retention - 12%
- Suture line bleeding- 4%
- Anastomotic leak- 3%
- Clostridium difficile colitis - 3%
- Anastomotic stricture - 1%
- Recurrence rate - 14.5% at a mean time of 31 months
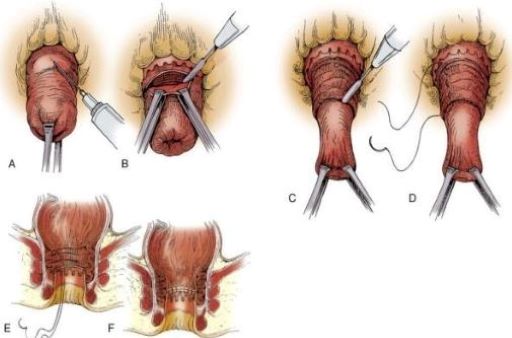
Altemeier procedure
In 1889, Mikulicz first described the procedure but it was popularized in 1971by Altemeier.
Perineal approach.
*Full thickness resection of rectum and a portion of sigmoid colon (procto-sigmoid colectomy) are done and anastomosis is performed using absorbable sutures.
*Simultaneous anterior levatorplasty is also performed to prevent fecal incontinence.
*The entire procedure can be completed now by using the surgical stapling devices.
The recurrence rate reported by Altemeier was 3.5%
ABDOMINAL PROCEDURES FOR RECTAL PROLAPSE
RECROPEXY (fixation) PROCEDURES
- Sigmoidopexy (Pemberton Stalker)
- Presacral Rectopexy
- Lateral strip rectopexy (Orr-Loygue)
- Anterior sling rectopexy (Wells)
- Puborectal sling
- Suture rectopexy (Cutait)
RESECTION PROCEDURES
- Rectopexy with sigmoid resection(Frykman Goldberg procedure)
- Anterier resection
Repair of pelvic floor
- Repair of Levator diastasis
- Abdominoperineal levator repair
Well's Procedure
- Posterior mesh rectopexy
- in Posterior rectopexy, the mesh is placed between the mobilized rectum and the sacrum.
- It is then fixed to the sacral fascia by sutures. Instead of using an ivalon (polyvinyl alcohol)
- A polypropelene or a polyster mesh is used in the Modefied Well's technique
- This technique is very useful particularly for the laparoscopic repair. With a low recurrence rate 0% to 6% and low mortality rate 0% to 3%.

Ripstein procedure
Resection-Rectopexy - (Frykman-Goldberg Procedure)
Principle
- Upper rectum plus redundant sigmoid colon is resected & re-anastomosed.
- Rectum is fixed to the presacral fascia with sutures.
Advantages
- Low morbidity & mortally of 0-6.5%
- Low recurrence rate of 0-5%